CHARLOTTE AMALIE — Some healthcare workers are pushing back against new mandates requiring employees to be vaccinated against COVID-19, but Schneider Hospital CEO Dr. Luis Amaro said such mandates are nothing new, and are the best way for physicians and nurses to keep their patients safe.
Amaro said in an interview with The Daily News yesterday that hospital workers have long been required to show proof of vaccination against a variety of illnesses, including hepatitis B, measles, mumps, rubella, tetanus, and varicella, commonly known as chickenpox.
The Virgin Islands Health and Hospital Facilities Corporation recently issued a similar order requiring all Virgin Islands hospital staff to show proof of COVID-19 vaccination, and estimated that only 55 percent of hospital staff have received at least one dose of the vaccine.
“It’s certainly not enough. We need to get at least over 80 percent, and now we’re going to get over 100 percent, and that’s what’s protective to the community,” Amaro said. “Our healthcare staff are heroes, they are the backbone of what we do to protect this community. But this measure is another tool to protect this community, inclusive of the skills and talents of the staff.”
Government House Communications Director Richard Motta did not respond to requests for comment.
Schneider and Luis hospitals “join 123 other hospitals, plus two states — New York and California — in requiring vaccination for healthcare workers,” according to a news release issued Sunday by Luis Hospital attorney Chivonne Thomas, in response to questions from The Daily News. “Keeping skilled local nurses and employees is a top priority for JFL. The goal of the vaccine mandate is not to exclude anyone, but to ensure the safety of staff and patients and the overall community.”
Amaro said weekly COVID-19 testing is not being provided as an alternative to vaccination because it can take 48 to 72 hours for symptoms to appear after infection, and asymptomatic spreaders can infect coworkers and patients for days before testing positive.
He also explained that the travel portal is no longer accepting antibody tests because the tests can’t differentiate between previous COVID-19 infection and vaccination. While vaccination protects against a variety of COVID-19 variants, previous infection provides immunity against only the strain that caused the illness, and does not offer protection against reinfection with other COVID-19 variants, Amaro said.
Hospital staff will only receive a waiver from the new mandate if they can show proof of a deeply held religious belief that prohibits them from being vaccinated, or have a documented medical “contraindication” or allergy to vaccines. Such exemptions will be evaluated on a “case-by-case basis,” Amaro said, and staff who do not comply with the vaccine or testing mandate will face termination.
Amaro said employment at a public hospital is conditional because staff must be held to a standard of quality that will ensure patient safety and limit liability.
“It goes along with making sure the staff is trained, that they’re credentialed,” Amaro said. “Part of that is making sure that they’re vaccinated. Vaccination is no different than credentialing, it’s no different than any of these other measures. You can’t choose not to be credentialed in the field you’re working in.”
The Luis Hospital news release refuted several statements posted online about the hospital’s operations, including a claim that hospital workers have not received hazard pay for treating COVID-19 patients: “All employees with direct patient care responsibilities to COVID-19 patients receive a COVID-19 differential.”
There are also rumors that the government is shipping in healthcare workers to replace unvaccinated local employees, but Amaro said the hospitals’ chronic staffing shortages predate the vaccine mandate.
“Both hospitals have been engaged in bringing in staffing for the sole purpose of providing relief to our understaffed situation. There was never any intent in replacing unvaccinated staff,” Amaro said. If the hospitals continue to suffer shortages for any reason, “then we would have to use emergency back up staffing to fill in.”
Hospitals have been under enormous strain in dealing with a recent, ongoing spike in COVID-19 cases.
Amaro said there are currently 10 COVID-19 patients admitted at Schneider Hospital, and five of those are on ventilators. As of Sunday, 16 COVID-19 patients were receiving treatment at Luis Hospital, including three on ventilators.
Those numbers remain “very concerning,” Amaro said.
All of the 40 people who have died of COVID-19 and all of those hospitalized with the disease in the territory were unvaccinated.
“This pandemic is a major health crisis and healthcare professionals and our dedicated JFL staff have led the way in the Territory’s response. It is our responsibility to lead in recovery and eradication of COVID-19 through vaccination,” Interim Luis Hospital CEO Dyma Williams said in a statement Sunday.
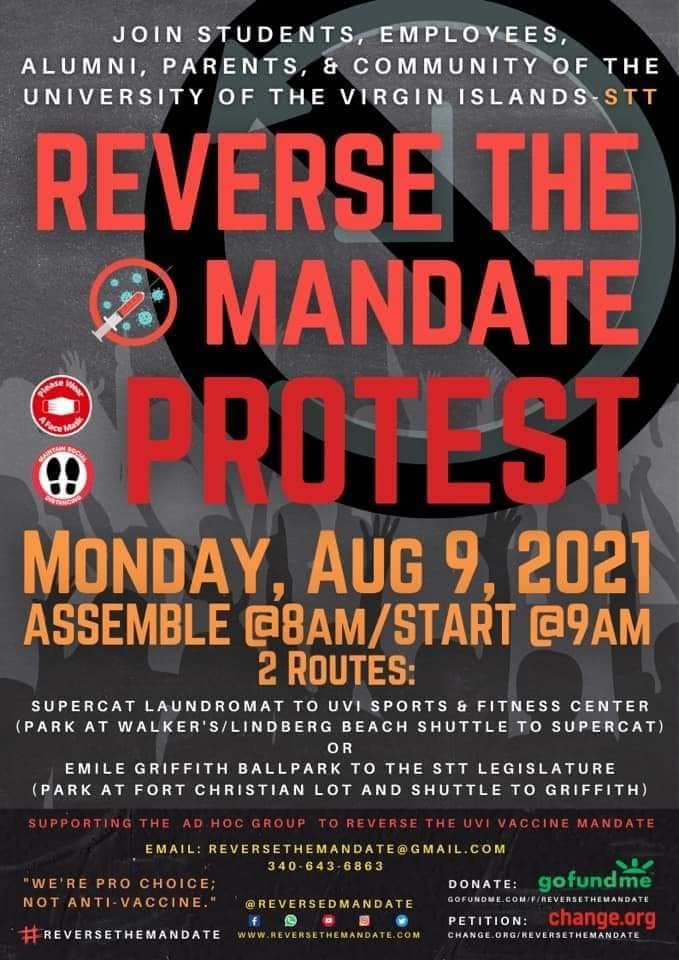
A vaccine mandate for University of the Virgin Islands staff prompted a protest planned for today at the St. Thomas campus, and some staff at Luis Hospital are expected to protest the vaccine mandate Tuesday on St. Croix.
Amaro said he spoke with staff at Schneider Hospital on Friday and heard from employees concerned about the vaccine.
One worry is the emergency approval, as opposed to other vaccines vetted by the traditional Food and Drug Administration process.
Many vaccines were approved decades ago and “in today’s testing, and what is being done, so much more is being done today to check the validity of a vaccine,” Amaro said. “And right now, as the evidence sits, it’s so heavily weighted in the success. You may get adverse reactions like fevers and chills like you do any other vaccine, but you’re not seeing the complications of death compared to the actual infection.”
Handwashing, masking, and social distancing were considered best practices before the vaccine was available, but vaccination is now humanity’s best chance at stopping infections from spreading, so “now we have to adopt that. That’s our responsibility as a healthcare institution for the patients that we treat,” he said.
He asked employees to think about one of their loved ones who might need to be hospitalized, and how they would feel if that person got COVID-19 from a staff member and died.
Some responded that vaccinated people could still spread the virus.
While Amaro said that is “partially true” and breakthrough infections are possible with the delta variant, “the transmission of COVID in a vaccinated individual is infinitesimally lower than that of an unvaccinated individual.”
Just like a medical license gives patients confidence that healthcare professionals have the skills to do their jobs safely, vaccine mandates give patients confidence that they’ll be safe from COVID-19 infection while they’re being treated in public hospitals.
“In 10, 15, or 20 years, if there’s another disease that comes about that becomes as huge public health concern that’s not going away, and there’s a vaccination for that, we will add that to the list. Whatever it is to protect the community, that is what’s most important,” Amaro said. “We make choices when we go into different fields. Whether we go into the military, public office, or healthcare, you have to meet the muster to perform in those fields.”
By SUZANNE CARLSON/The Virgin Islands Daily News