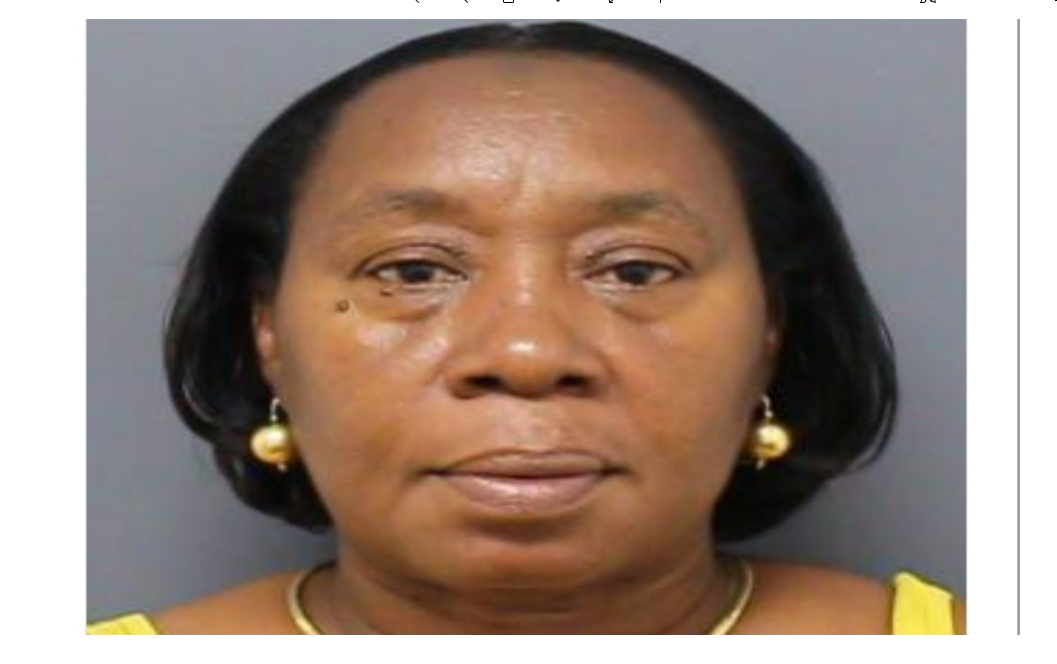
CHARLOTTE AMALIE — Virgin Islands Attorney General Denise George today announced the arrest of Department of Human Services employee Edith Brathwaite of St. Thomas.
Brathwaite was arrested by the Medicaid Fraud Control Unit (MFCU) of the Virgin Islands Department of Justice (VIDOJ) for allegedly defrauding the Virgin Islands Medicaid program, according to Attorney General George.
The arrest arose from a joint fraud investigation by the MFCU, the V.I. Inspector General’s Office and the federal Department of Health and Human Services Office of the Inspector General (HHS-OIG). The Virgin Islands Medicaid Fraud Control Unit is 100 percent federally funded and one of 53 Medicaid Fraud Control Units created by Congress specifically to investigate fraud, waste, and abuse in the local Medicaid programs.

At the time of the alleged crime, Brathwaite was employed as an Eligibility Specialist I with the Virgin Islands Medicaid Program, under the Virgin Islands Department of Human Services (DHS) and received government employee health insurance benefits.
Brathwaite was arrested on a Superior Court warrant charging her with violations of the V.I. Medicaid Fraud statute, fraudulent claims upon the government, conversion of government property, embezzlement, or falsification of public records, obtaining money by false pretenses, and grand larceny, for allegedly falsifying her income information on a hospital document to a lower amount in order to qualify for presumptive Medicaid benefits of which she knew was not lawfully eligible.
The investigation began in February of 2020 when the MFCU received an anonymous complaint alleging that several employees of the Virgin Islands Medicaid Program were defrauding the Medicaid program by fraudulently granting Medicaid benefits to themselves, family members, persons living outside of the United States, and their friends.
The investigation revealed that some employees of the Virgin Islands Medicaid Program were under-reporting their income in order to obtain Medicaid benefits. In some instances, the employees worked on each other’s Medicaid case and failed to report income when the income, if reported, would have disqualified the employees/applicants for benefits. In other cases, employees attempted several income levels until they arrived at the levels that would qualify their co-workers for benefits.
Employees enrolled undocumented persons, who are not entitled to Medicaid benefits, in the Medicaid program and continued to grant Medicaid benefits to family and friends living outside of the United States. And, in other instances, employees were issued forced eligibility in order for their co-workers whose income exceeded the Medicaid income level, to qualify for benefits. Brathwaite is one of three employees that have been arrested thus far. The investigation revealed that all employees were covered under the Government Health Insurance and were using Medicaid to pay for their co-pay.
It is alleged that on January 19, 2019, Brathwaite went to the emergency room at the Schneider Regional Medical Center in St. Thomas for medical attention. Braithwaite was subsequently admitted to the hospital for medical treatment. At some point during her stay at the hospital, Brathwaite was approached by hospital Employee #1 about filling out a Hospital Presumptive Eligibility (HPE) for medical benefits under the Virgin Islands Medicaid program. Based on their conversation, Brathwaite and the hospital Employee #1 knew then that Brathwaite would not be eligible for Medicaid benefits due to her income. So, she did not complete an HPE application.
The Virgin Islands Medicaid program allows an individual who is being seen at the emergency room at a local hospital to complete a HPE application to obtain Medicaid benefits. The applicant is not required to sign the application nor to provide any verification of income. Once the HPE application process is completed, the applicant is determined to be “presumptively eligible” for Medicaid benefits.
Consequently, the hospital may invoice the Medicaid program for services provided to the individual and the hospital will receive payments for services provided to the individual during the 60-day period. Once the HPE expires, the individual is required to submit further documentation including income to the Medicaid program to obtain Medicaid benefits.
It is alleged that Brathwaite was released from the hospital on January 22, 2019. And, on February 1, 2019, Brathwaite went to SRMC and requested to speak with hospital Employee #1. Brathwaite completed an HPE application for submittal. Brathwaite stated an income level that would have made her ineligible for Medicaid benefits.
But hospital Employee #1 informed Brathwaite that at that income level she would not qualify for Medicaid benefits. Brathwaite crossed out the income level and entered a lower amount that was false. Based on that amount, she was qualified for benefits and the hospital was able to invoice the Virgin Islands Medicaid program for the services that Brathwaite received during her stay at SRMC.
Medicaid is a multi-billion-dollar joint state and federal program that provides health coverage for
the economically disadvantaged. It provides essential medical care to low-income Virgin Islanders
including children. Medicaid fraud impacts the most vulnerable in our community and can place
millions of dollars in federal funds to VI in jeopardy. It costs American taxpayers an incalculable
amount of money and hinders the integrity of the Medicaid program. Medicaid Fraud Control
Units have long been the vehicle used to enforce health care fraud. However, in 1995, Congress
enacted legislation that requires each state to have a Medicaid Fraud Control Unit or submit a
waiver to the Secretary of the US Department of Health and Human Services.
The Virgin Islands Medicaid Fraud Control Unit is 100 percent federally funded and one of 53 Medicaid
Fraud Control Units created by Congress specifically to investigate fraud, waste, and abuse in the
Medicaid programs. The Virgin Islands Medicaid Fraud Control Unit is 100 percent funded by a grant from the DHH-OIG and works cooperatively with the Virgin Islands Department of Human Services and other territorial and federal partners to prosecute fraud in the Virgin Islands Medicaid program.
“My office remains dedicated to protecting taxpayers’ dollars and pursuing potential instances of Medicaid fraud and corruption,” AG Denise George said. “Through our Medicaid Fraud Control Unit, we work diligently to meet our mandate and uphold the integrity of the Virgin Islands Medicaid program and hold those accountable who would abuse the public trust.”
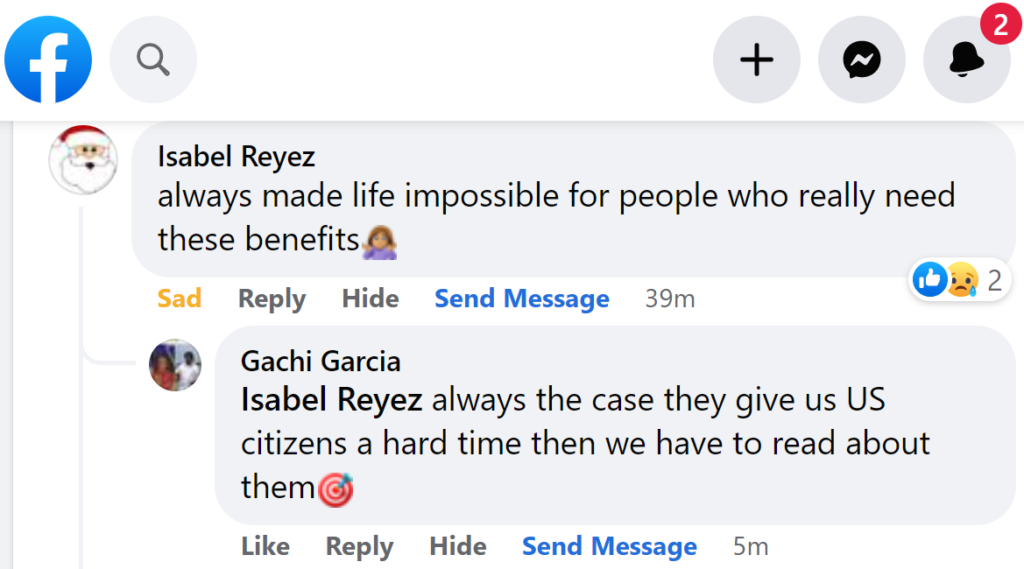
People on social media were harshly critical of Brathwaite and the “bad attitude” of Human Services’ employees in general.
“Always made life impossible for people who really need these benefits,” Isabel Reyez said on Facebook.
“Isabel Reyez always the case they give us U.S. citizens a hard time then we have to read about them,” Gachi Garcia replied to Isabel Reyez.
“Isabel Reyez exactly. When people go with all the documents needed they are deny,” Avlyn Romain replied to Isabel Reyez.
“Bless her those people probably needed it and even if they didn’t she was giving what she had, which is a human right,” Tay Boo said from St. Thomas.
“That’s how things are done here. It’s all about family and friends. Lovely!” Tetyana Hayes said.
“She handle my bbm case an drop it to 25 dollars case she added some paper that wasn’t belongs to add.. funny how the tables have turn. You look like you could use that 25dollars right about now ..” Franky Green said.
On social media, Ms. Brathwaite said she attended Charlotte Amalie High School (CAHS) on St. Thomas.
AG George cautions the public that in a court of law, any person charged with a crime in the Virgin
Islands is innocent until proven guilty.